Thalidomide
 | |
|---|---|
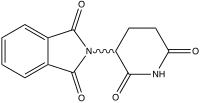
| Systematic (IUPAC) name | |
| (RS)-2-(2,6-dioxopiperidin-3-yl)-1H-isoindole-1,3(2H)-dione | |
| Identifiers | |
| CAS number | 50-35-1 |
| ATC code | L04AX02 |
| PubChem | CID 5426 |
| DrugBank | DB01041 |
| ChemSpider | 5233 |
| UNII | 4Z8R6ORS6L |
| KEGG | D00754 |
| ChEMBL | CHEMBL468 |
| Chemical data | |
| Formula | C13H10N2O4 |
| Mol. mass | 258.23 g/mol |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Protein binding | 55% and 66% for the (+)-R and (–)-S enantiomers, respectively |
| Metabolism | Hepatic (CYP2C19) |
| Half-life | mean ranges from approximately 5 to 7 hours following a single dose; not altered with multiple doses |
| Therapeutic considerations | |
| Pregnancy cat. | X(AU) X(US) |
| Legal status | ℞ Prescription only |
| Routes | oral |
| | |
Thalidomide (![]() /θəˈlɪdəmaɪd/) was introduced as a sedative drug in the late 1950s. In 1961, it was withdrawn due to teratogenicity and neuropathy. There is now a growing clinical interest in thalidomide, and it is introduced as an immunomodulatory agent used primarily, combined with dexamethasone, to treat multiple myeloma. The drug is a potent teratogen in zebrafish, chickens, rabbits and primates including humans: severe birth defects may result if the drug is taken during pregnancy.
/θəˈlɪdəmaɪd/) was introduced as a sedative drug in the late 1950s. In 1961, it was withdrawn due to teratogenicity and neuropathy. There is now a growing clinical interest in thalidomide, and it is introduced as an immunomodulatory agent used primarily, combined with dexamethasone, to treat multiple myeloma. The drug is a potent teratogen in zebrafish, chickens, rabbits and primates including humans: severe birth defects may result if the drug is taken during pregnancy.
Thalidomide was sold in a number of countries across the world from 1957 until 1961 when it was withdrawn from the market after being found to be a cause of birth defects in what has been called "one of the biggest medical tragedies of modern times". It is not known exactly how many worldwide victims of the drug there have been, although estimates range from 10,000 to 20,000. Since then thalidomide has been found to be a valuable treatment for a number of medical conditions and it is being prescribed again in a number of countries, although its use remains controversial, including its testing in the developing world. The thalidomide tragedy led to much stricter testing being required for drugs and pesticides before they can be licensed.
History
Development
Thalidomide was developed by German pharmaceutical company Grünenthal in Stolberg (Rhineland) near Aachen, although this claim has recently been challenged. A report published by Martin W. Johnson, director of the Thalidomide Trust in the United Kingdom, mentioned evidence found by Argentinian author Carlos De Napoli that suggested the drug had been first developed as a possible antidote to nerve toxins, such as Sarin, by Otto Ambros, a Nazi scientist who joined Grünenthal after the war. Correspondence between various drug companies, French firm Rhône-Poulenc, which was under Nazi control during the war years, Astra AB, which held the Swedish licence to distribute thalidomide, and IG Farben, the German pharmaceutical firm, seem to confirm the existence of the product years before Grünenthal secured a patent in 1954. Furthermore, a relation has been suggested between testing thalidomide and the Nazi death camps. Grünenthal has reacted to these claims by stating: “To our knowledge there was no collaboration between Grünenthal and Rhône-Poulenc for the development of Contergan/thalidomide. Three Grünenthal employees discovered thalidomide and Grünenthal is the sole inventor on the patent.” According to Grünenthal, Dr. Heinrich Mückter was one of those responsible for inventing Thalidomide. Other sources mark Dr. Mückter as a fledgling pharmacologist who carried out wartime experiments on Polish prisoners to find a cure for typhus. He caused the death of hundreds in the process.
De Napoli suggested elsewhere that thalidomide may have been first synthesised by British scientists at the University of Nottingham in 1949. Thalidomide, launched by Grünenthal on 1 October 1957, was found to act as an effective tranquiliser and painkiller and was proclaimed a "wonder drug" for insomnia, coughs, colds and headaches. It was also found to be an effective antiemetic which had an inhibitory effect on morning sickness, and so thousands of pregnant women took the drug to relieve their symptoms. At the time of the drug's development it was thought unlikely that any drug could pass from the mother across the placental barrier and harm the developing foetus. The Food and Drug Administration of the United States never licensed thalidomide for general use; according to Time Magazine, "In the half dozen reported U.S. cases of birth malformations due to thalidomide, the drug was obtained from abroad."
Birth defects
In the late 1950s and early 1960s, more than 10,000 children in 46 countries were born with deformities such as phocomelia, as a consequence of thalidomide use. The Australian obstetrician William McBride and the German pediatrician Widukind Lenz suspected a link between birth defects and the drug, and this was proved by Lenz in 1961. McBride was later awarded a number of honours including a medal and prize money by the prestigious L'Institut de la Vie in Paris.
In the United Kingdom the drug was licensed in 1958 and, of the approximately 2000 babies born with defects, 466 survived. The drug was withdrawn in 1961 and in 1968, after a long campaign by The Sunday Times newspaper, a compensation settlement for the UK victims was reached with Distillers Company Limited. In Germany approximately 2,500 thalidomide babies were born. In some extreme cases, it could kill the patient if there were other diseases or drugs in the body.
The impact in the United States was minimized when pharmacologist and M.D. Frances Oldham Kelsey refused Food and Drug Administration (FDA) approval for an application from the Richardson-Merrell company to market thalidomide, saying further studies were needed. And although thalidomide was never approved for sale in the United States, millions of tablets had been distributed to physicians during a clinical testing program. It was impossible to know how many pregnant women had been given the drug to help alleviate morning sickness or as a sedative.
Canada was the last country to stop the sales of the drug, in early 1962.
In 1962, the United States Congress enacted laws requiring tests for safety during pregnancy before a drug can receive approval for sale in the U.S. Other countries enacted similar legislation, and thalidomide was not prescribed or sold for decades.
September 2010, as noted in an article titled "The Public’s Quiet Savior From Harmful Medicine", the FDA honored Dr. Kelsey with the first Kelsey award. It will be given to an FDA staff member annually. The award came 50 years after Dr. Kelsey, then a new medical officer at the agency, first reviewed the application from the William S. Merrell Company of Cincinnati.
Mechanism
It was soon discovered that only one particular optical isomer of thalidomide caused the teratogenicity. The pair of enantiomers, while mirror images of each other, cause different effects, although it is now known that the "safe" isomer can be converted to the teratogenic isomer once in the human body.(see Teratogenic mechanism).
Revived interest
In 1964 Jacob Sheskin, Professor at the Hebrew University of Jerusalem at Hadassah University Hospital (he was also the chief staff and manager of Hansen Leper Hospital in Jerusalem), administered thalidomide to a critically ill patient with erythema nodosum leprosum (ENL), a painful complication of leprosy, in an attempt to relieve his pain in spite of the ban. The patient slept for hours, and was able to get out of bed without aid upon awakening. The result was followed by more favorable experiences and then by a clinical trial. He found that patients with erythema nodosum leprosum, a painful skin condition, experienced relief of their pain by taking thalidomide.
Further work conducted in 1991 by Dr. Gilla Kaplan at Rockefeller University in New York City showed that thalidomide worked in leprosy by inhibiting tumor necrosis factor alpha and believed it would be an effective treatment for AIDS. Kaplan partnered with Celgene Corporation to further develop the potential for thalidomide in AIDS and tuberculosis. However, clinical trials for AIDS proved disappointing.
In 1994, Dr. Robert D'Amato at Harvard Medical School discovered that thalidomide was a potent inhibitor of new blood vessel growth (known as angiogenesis). Numerous cancer clinical trials were initiated with thalidomide based upon this finding and subsequently in 1997 Dr. Bart Barlogie’s reported thalidomide’s initial effectiveness against Multiple Myeloma and it was later approved in the United States by the FDA for use in this malignancy. The FDA has also approved the drug's use in the treatment of erythema nodosum leprosum. There are studies underway to determine the drug's effects on arachnoiditis and several types of cancers. However, physicians and patients alike must go through a special process to prescribe and receive thalidomide (S.T.E.P.S.) to ensure no more children are born with birth defects traceable to the medication. Celgene Corporation has also developed analogues to thalidomide, such as lenalidomide, that are substantially more powerful and have fewer side effects — except for greater myelosuppression.
More recently the World Health Organisation (WHO) has stated that:
United States
On July 16, 1998, the FDA approved the use of thalidomide for the treatment of lesions associated with Erythema Nodosum Leprosum (ENL). Because of thalidomide’s potential for causing birth defects, the distribution of the drug was permitted only under tightly controlled conditions. The FDA required that Celgene Corporation, which planned to market thalidomide under the brand name Thalomid, establish a System for Thalidomide Education and Prescribing Safety (S.T.E.P.S.) oversight program. The conditions required under the program include; limiting prescription and dispensing rights only to authorized prescribers and pharmacies, keeping a registry of all patients prescribed thalidomide, providing extensive patient education about the risks associated with the drug and providing periodic pregnancy tests for women who are prescribed it. On May 26, 2006, the U.S. Food and Drug Administration granted accelerated approval for thalidomide (Thalomid, Celgene Corporation) in combination with dexamethasone for the treatment of newly diagnosed multiple myeloma (MM) patients. The FDA approval came seven years after the first reports of efficacy in the medical literature and Celgene took advantage of "off-label" marketing opportunities to promote the drug in advance of its FDA approval for the myeloma indication. Thalomid, as the drug is commercially known, sold over $300 million per year, while only approved for leprosy.
United Kingdom
Thalidomide is available to only a small number of patients in the UK, generally in specialist cancer treatment centres where research trials are taking place and specialist doctors have experience in its use.
Brazil
Brazil has the second highest prevalence rate of leprosy in the world and thalidomide has been used by Brazilian physicians as the drug of choice for the treatment of severe ENL since 1965. A study published in 1996 reported 33 people born in Brazil after 1965 with thalidomide embryopathy. Since 1994 the production, dispensing and prescription of thalidomide have been strictly controlled, but cases of thalidomide embryopathy are thought to have occurred until today.
Possible indications
Serious infections including sepsis and tuberculosis cause the level of Tumor necrosis factor-alpha (TNFα) to rise. TNFα is a chemical mediator in the body, and it may enhance the wasting process in cancer patients as well. Thalidomide may reduce the levels of TNFα, and it is possible that the drug's effect on ENL is caused by this mechanism.
Thalidomide also has potent anti-inflammatory effects that may help ENL patients. In July 1998, the FDA approved the application of Celgene to distribute thalidomide under the brand name Thalomid for treatment of ENL. Pharmion Corporation, who licensed the rights to market thalidomide in Europe, Australia and various other territories from Celgene, received approval for its use against multiple myeloma in Australia and New Zealand in 2003. Thalomid, in conjunction with dexamethasone, is now standard therapy for multiple myeloma.
Thalidomide is also prescribed for its anti-inflammatory effects in actinic prurigo, an autoimmune skin disease. Thalidomide has been used in chronic bullous dermatosis of childhood (CBDC) with encouraging results. Although, peripheral neuritis may be a limiting factor for long term use of thalidomide.
Thalidomide also inhibits the growth of new blood vessels (angiogenesis), which may be useful in treating macular degeneration and other diseases. This effect helps AIDS patients with Kaposi's sarcoma, although there are better and cheaper drugs to treat the condition. Thalidomide may be able to fight painful, debilitating aphthous lesions in the mouth and esophagus of AIDS patients which prevent them from eating. The FDA formed a Thalidomide Working Group in 1994 to provide consistency between its divisions, with particular emphasis on safety monitoring. The agency also imposed severe restrictions on the distribution of Thalomid through the System for Thalidomide Education and Prescribing Safety (STEPS) program.
Thalidomide is also being investigated for treating symptoms of prostate cancer, glioblastoma, lymphoma, arachnoiditis, Behçet's disease, and Crohn's disease. In a small trial, Australian researchers found thalidomide sparked a doubling of the number of T cells in patients, allowing the patients' own immune system to attack cancer cells.
Studies carried out in animal models have suggested that the use of combined therapy with thalidomide and glucantime could have a therapeutic benefit in the treatment of *Visceral Leshmaniasis.
A study published in April 2010 discusses the ability of thalidomide to induce vessel maturation, which may be useful as a therapeutic strategy for the treatment of vascular malformations. The research was conducted in an experimental model of the genetic disease hereditary hemorrhagic telangiectasia.
Thalidomide and multiple myeloma
Thalidomide was first tested in humans as a single agent for the treatment of multiple myeloma in 1996 due to its antiangiogenic activity and the full study published in 1999. Since then many studies have shown that thalidomide in combination with dexamethasone has increased the survival of multiple myeloma patients. The combination of thalidomide and dexamethasone, often in combination with melphalan, is now one of the most common regimens for patients with newly diagnosed multiple myeloma, with an improved response rate of up to 60-70%. Thalidomide may also cause side effects such as polyneuropathy, fatigue, skin rash, and venous thromboembolism (VTE), or blood clots, which could lead to stroke or myocardial infarction. Bennett et al. have conducted a systematic review of VTE associated with thalidomide in multiple myeloma patients. They have found that when thalidomide was administered without prophylaxis, VTE rates reached as high as 26%. Owing to the high rates of VTE associated with thalidomide in combination with dexamethasone or doxorubicin, a black box warning was added in the US in 2006 to the package insert for thalidomide, indicating that patients with multiple myeloma who receive thalidomide-dexamethasone may benefit from concurrent thromboembolism prophylaxis or aspirin. In addition, owing to these side effects, newer drugs, such as bortezomib (marketed as Velcade) and a thalidomide derivative, lenalidomide (marketed as Revlimid), have increased in popularity.
Teratogenic mechanism
Thalidomide is racemic – it contains both left- and right-handed isomers in equal amounts. The (R) enantiomer is effective against morning sickness but the (S) is teratogenic. The enantiomers can interconvert (racemize) in vivo – that is, if a human is given pure (R)-thalidomide or (S)-thalidomide, both isomers will later be found in the serum – therefore, administering only one enantiomer will not prevent the teratogenic effect.
The mechanism of thalidomide's teratogenic action has led to over 2000 research papers and the proposal of fifteen or sixteen plausible mechanisms. A theoretical synthesis in 2000 suggested the following mechanism: thalidomide intercalates (inserts itself) into DNA in G-C (guanine-cytosine) rich regions. Owing to its glutarimide part, (S) thalidomide fits neatly into the major groove of DNA at purine sites. Such intercalation impacts upon the promoter regions of the genes controlling the development of limbs, ears, and eyes such as IGF-I and FGF-2. These normally activate the production of the cell surface attachment integrin αvβ3 with the resulting αvβ3 integrin dimer stimulating angiogenesis in developing limb buds. This then promotes the outgrowth of the bud (IGF-I and FGF-2 are also both known to stimulate angiogenesis). Therefore, by inhibiting the chain of events, thalidomide causes the truncation of limb development. In 2009 this theory received strong support, with research showing "conclusively that loss of newly formed blood vessels is the primary cause of thalidomide teratogenesis, and developing limbs are particularly susceptible because of their relatively immature, highly angiogenic vessel network."
Inactivation of the protein cereblon
Thalidomide binds to and inactivates the protein cereblon, which is important in limb formation. The inactivation, thus, leads to a teratogenic effect on fetal development. This was confirmed when the scientists, using genetic techniques, reduced the production of cereblon in developing chick embryo and zebrafish embryo. These embryos had defects similar to those treated with thalidomide. Thus the mechanism that causes teratogenicity has been established but the mechanism for other therapeutic effects remains unclear.
Thalidomide analogs
The exploration of the antiangiogenic and immunomodulatory activities of thalidomide has led to the study and creation of thalidomide analogs. In 2005, Celgene received FDA approval for lenalidomide (Revlimid) as the first commercially useful derivative. Revlimid is only available in a restricted distribution setting to avoid its use during pregnancy. Further studies are being conducted to find safer compounds with useful qualities. Another analog, pomalidomide, is in the clinical trial phase. These thalidomide analogs can be used to treat different diseases, or used in a regimen to fight two conditions.
Notable people affected
References
Further reading
External links
- Thalidomide monograph from Chemical and Engineering News. (Archived by WebCite® at http://www.webcitation.org/5nWHyOCfI)
- Thalidomide product monograph (Needs registration)
- Multiple Myeloma Research Foundation article on Thalidomide
- International Myeloma Foundation article on Thalidomide
- Thalidomide — Annotated List of Links (covering English and German pages)
- WHO Pharmaceuticals Newsletter No. 2, 2003 - See page 11, Feature Article
- Grünenthal GmbH - Thalidomide
- Celgene website on Thalomid
- The Return of Thalidomide - BBC
- CBC Digital Archives – Thalidomide: Bitter Pills, Broken Promises
- Thalidomide UK
- The Thalidomide Trust
- The International Contergan Thalidomide Alliance website
- "The Big Pitch: How would you conduct a campaign for the new Thalidomide Drugs?", forum of pharmaceutical and medical marketing professionals commenting on how they would address the thalidomine controversies.
Retrieved from : http://en.wikipedia.org/wiki/Thalidomide